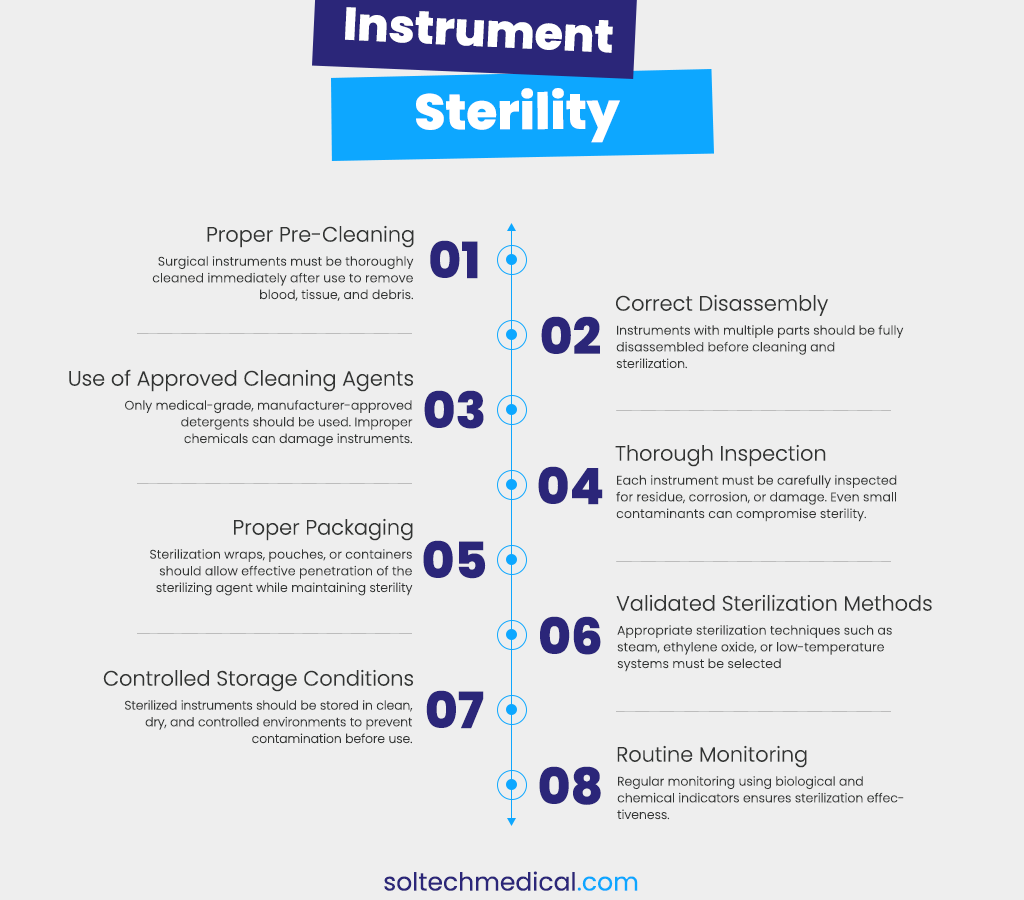
8 Essential Steps to Maintain Surgical Instrument Sterility
In surgery, sterility is not optional — it is fundamental. Every surgical instrument that enters an operating room carries responsibility: the safety of the patient, the confidence of the surgeon, and the integrity of the procedure itself. Maintaining surgical instrument sterility requires more than just advanced equipment; it depends on consistent practices, attention to detail, and a strong understanding of each step in the sterilization process.
Below are eight essential steps that help ensure surgical instruments remain safe, sterile, and ready for use.
- Proper Pre-Cleaning
Sterility begins immediately after a procedure ends. Instruments must be pre-cleaned as soon as possible to remove blood, tissue, and organic debris. When contaminants are allowed to dry, they become harder to remove and can block sterilizing agents from reaching critical surfaces. Early cleaning not only improves sterilization effectiveness but also protects the lifespan of the instrument.
- Correct Disassembly
Many modern surgical instruments are designed with multiple components, hinges, or lumens. These areas can trap debris if instruments are not fully disassembled before cleaning. Proper disassembly ensures that all surfaces — visible and hidden — are accessible, allowing thorough cleaning and reliable sterilization.
- Use of Approved Cleaning Agents
Not all cleaning solutions are suitable for surgical instruments. Using unapproved or harsh chemicals can damage metal surfaces, reduce sharpness, and compromise long-term performance. Medical-grade detergents specifically designed for surgical instruments are formulated to clean effectively while preserving material integrity and functionality.
- Careful Inspection Before Sterilization
Before instruments move forward in the sterilization process, they must be carefully inspected. Traces of residue, corrosion, stains, or mechanical damage can indicate incomplete cleaning or instrument wear. Identifying and addressing these issues early helps prevent contamination risks and ensures instruments function properly during surgery.
- Proper Packaging and Wrapping
Packaging plays a critical role in maintaining sterility after processing. Sterilization wraps, pouches, or rigid containers must allow sterilizing agents to penetrate fully while protecting instruments from contamination during storage and transport. Incorrect packaging can compromise even the most effective sterilization cycle.
- Validated Sterilization Methods
Different instruments require different sterilization techniques depending on their material and design. Steam sterilization is widely used for heat-resistant instruments, while low-temperature methods are preferred for delicate or heat-sensitive tools. Following validated sterilization protocols ensures consistent, reliable results without damaging instruments.
- Controlled Storage Conditions
Sterilization does not end when instruments leave the sterilizer. Sterile instruments must be stored in clean, dry, and controlled environments to prevent recontamination. Proper shelving, airflow control, and limited handling help preserve sterility until the moment instruments are needed in the operating room.
- Routine Monitoring and Documentation
Regular monitoring is essential to confirm that sterilization processes are working effectively. Chemical indicators, biological tests, and detailed documentation provide traceability and accountability. This step supports compliance with healthcare standards and builds confidence in the safety of every surgical procedure.